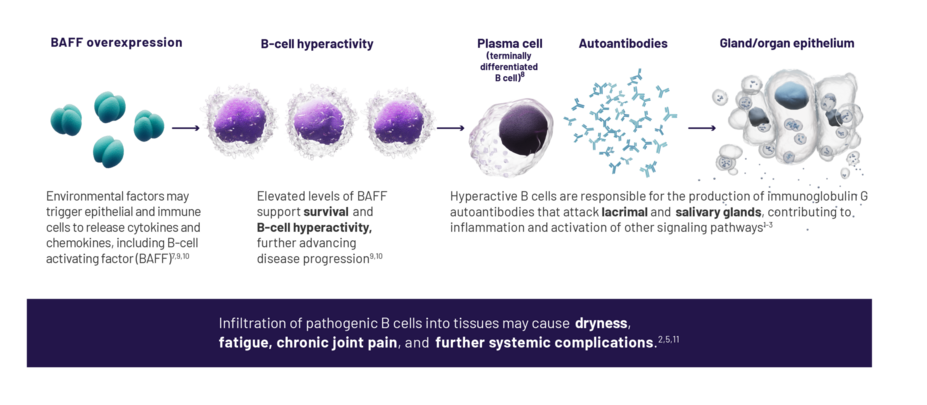
Sjögren's disease (SjD) is believed to be a B-cell–driven autoimmune disease in which the perpetual activation of B cells results in a pathological cycle of immune activation, leading to chronic inflammation and irreversible tissue destruction.1-4
Hyperactive B cells play a key role in systemic inflammation among patients with SjD1-3,5-8
In addition to B cells, other immune cells, such as T cells, also play a role in the pathogenesis of SjD, contributing to an autoimmune cascade and chronic inflammation.7,12
The mechanism of SjD
Novartis is committed to innovation in SjD
As current B-cell–targeted approaches have failed to demonstrate significant outcomes in SjD, several novel therapies for effective and sustained B-cell depletion are currently under investigation.14,15
Novartis has expanded its commitment to rheumatology by partnering with experts and universities to explore new ways to target B-cell hyperactivity and BAFF.
QOL, quality of life.
References: 1. Meng Q, Ma J, Cui J, Gu Y, Shan Y. Subpopulation dynamics of T and B lymphocytes in Sjögren’s syndrome: implications for disease activity and treatment. Front Immunol. 2024;15:1468469. doi: 10.3389/fimmu.2024.1468469 2. Du W, Han M, Zhu X, et al. The multiple roles of B cells in the pathogenesis of Sjögren’s syndrome. Front Immunol. 2021;12:684999. doi:10.3389/fimmu.2021.684999 3. Ibrahem HM. B cell dysregulation in primary Sjögren’s syndrome: a review. Jpn Dent Sci Rev. 2019;55(1):139-144. 4. Kroese F, Abdulahad WH, Haacke E, Bos NA, Vissink A, Bootsma H. B-cell hyperactivity in primary Sjögren’s syndrome. Expert Rev Clin Immunol. 2014;10(4):483-499. 5. Verstappen GM, Pringle S, Bootsma H, Kroese FGM. Epithelial–immune cell interplay in primary Sjögren syndrome salivary gland pathogenesis. Nat Rev Rheumatol. 2021;17(6):333-348. 6. Nocturne G, Mariette X. B cells in the pathogenesis of primary Sjögren syndrome. Nat Rev Rheumatol. 2018;14(3):133-145. 7. Chivasso C, Sarrand J, Perret J, Delporte C, Soyfoo MS. The involvement of innate and adaptive immunity in the initiation and perpetuation of Sjögren’s syndrome. Int J Mol Sci. 2021;22(2):658. doi:10.3390/ijms22020658 8. Witas R, Gupta S, Nguyen CQ. Contributions of major cell populations to Sjögren’s syndrome. J Clin Med. 2020;9(9):3057. doi:10:3390/jcm9093057 9. Parisis D, Chivasso C, Perret J, Soyfoo MS, Delporte C. Current state of knowledge on primary Sjögren's syndrome, an autoimmune exocrinopathy. J Clin Med. 2020;9(7):2299. doi:10.3390/jcm9072299 10. Nocturne G, Mariette X. Advances in understanding the pathogenesis of primary Sjögren's syndrome. Nat Rev Rheumatol. 2013;9(9):544-556. 11. Mariette X, Criswell LA. Primary Sjögren's syndrome. N Engl J Med. 2018;378(10):931-939. 12. Negrini S, Emmi G, Greco M, et al. Sjögren's syndrome: a systemic autoimmune disease. Clin Exp Med. 2022;22(1):9-25. 13. McCoy SS, Woodham M, Bunya VY, et at. A comprehensive overview of living with Sjögren's: results of a National Sjögren's Foundation survey. Clin Rheumatol. 2022;41(7):2071-2078. 14. Thalayasingam N, Baldwin K, Judd C, Ng WF. New developments in Sjögren's syndrome. Rheumatology (Oxford). 2021;60(suppl 6):vi53-vi61. 15. Ramos-Casals M, Brito-Zerón P, Bombardieri S, et al. EULAR recommendations for the management of Sjögren's syndrome with topical and systemic therapies. Ann Rheum Dis. 2020;79:3-18.